You never realize the extensive use and utility of shoulder joint until it starts hurting. It is the most mobile joint of our body which is extensively used in our activities of daily living. However mobility comes at the cost of stability. Shoulder pain can surface because of pathology in shoulder joint proper or muscles around it. It gets worse as you move the arm, lift weight or indulge in sports. Pain may be temporary or long lasting. It may get chronic if overlooked. At SAAOL Ortho Care we take an integrative approach to correctly diagnose the pinpoint source of shoulder pain and provide non-surgical treatment to help you get on a personalized path of optimum recovery. Contact us to keep your shoulders healthy, painless and moving.
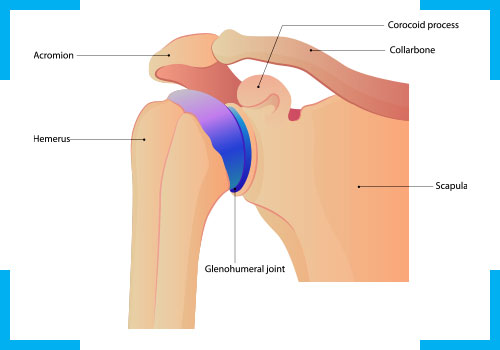
The shoulder joint (glenohumeral joint) is a ball and socket joint between the scapula and the humerus. It is the major structure connecting the upper limb to the trunk and is one of the most mobile joints in the human body. The rotator cuff is a collection of muscles (supraspinatus, infraspinatus, teres minor and subscapularis) and tendons that surround the shoulder, giving it support and allowing a wide range of motion. The bursa is a small sac of fluid that cushions and protects the tendons of the rotator cuff. A cuff of cartilage called the labrum forms a cup for the ball-like head of the humerus to fit into.
Include Degeneration (Tendinosis) or Inflammation (Tendinits) of Rotator Cuff Tendons. Supraspinatus muscle is most commonly involved. Degeneration and Inflammation occur due to overuse of these tendons and lead to Pain in posterolateral aspect of shoulder which is dull, aching and usually at night and when arm is abducted more than 90 degrees. Tested clinically or using Dynamic Ultrasonography or MRI, this condition can be managed holistically using medications, electrotherapy, manual therapy, exercises and PRP or anti-inflammatory injections.
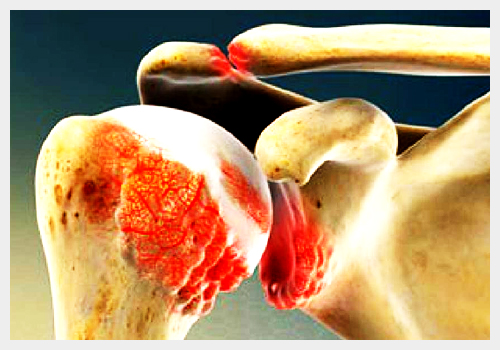
Characterized by loss of cartilage , narrowing of space , synovitis and osteophytes, this condition is typically seen in aged people with a history of shoulder overuse. Shoulder pain intensified by activity and partially relieved with rest and is usually noted with all shoulder movements. Pain is typically worse when supine and in attempting to sleep on the arthritic side with reduced range of motion and crepitations. Medications can help with pain and enable rehabilitation. Capsaicin cream, lidocaine patches, ice, or moist heat may be used topically as needed. Gentle stretching exercises help keep the range of motion and prevent secondary adhesive capsulitis. Aquatic rehab has huge benefit. Intra-articular Injections of Hyaluronic Acid and PRP can be used
Adhesive capsulitis of the shoulder is an idiopathic, progressive, but self-limited restriction of active and passive range of motion. The onset is insidious and progresses through three phases, usually during the course of 1 to 2 years. These phases include the painful phase, the freezing or adhesive phase, and the thawing or resolution phase. It is more common in women and from the age of 40-60 years. Your risk might also go up if you’re in the process of recovering from a medical condition like a stroke, or surgery like a mastectomy that keeps you from moving your arm. About 10% to 20% of people with diabetes get frozen shoulder. Other medical problems like heart disease, thyroid disease, or Parkinson’s disease are linked to frozen shoulder, too. Pain and inflammation should be managed by use of ice, anti-inflammatories, and activity modifications. Injections of corticosteroid (with or without lidocaine) into the subacromial space and/or Suprascapular nerve blocks are in many cases useful in breaking pain cycles.

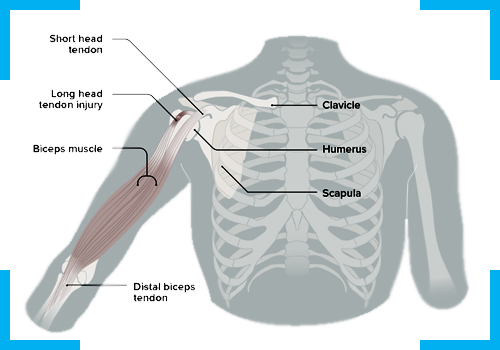
Isolated inflammation of the tendon as it runs in the intertubercular groove of humerus. Mostly seen in young/athletic population and in aged. Mostly it is associated with rotator cuff pathology. Characterized by anterior shoulder pain which occurs with shoulder flexion and lifting activities that involve elbow flexion. Medications with UST, PEMF, stretching and ROM exercises and PRP/Anti inflammatory injections are best treatment options.
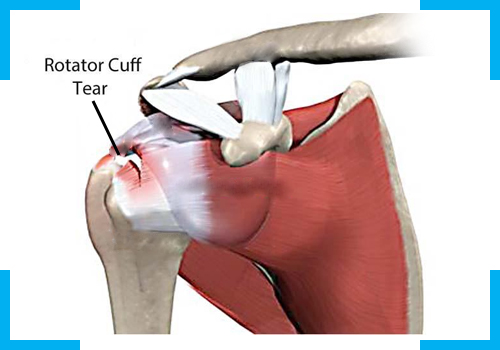
Two types of Tears can occur in Rotator cuff, full thickness tear or partial thickness tear. Mostly tears can be traumatic or degenerative. Both types can cause excruciating pain and functional impairments. Tears can be diagnosed by clinical tests, ultrasonography and MRI. Treatment includes medications, exercises, UST, PEMF, IFT and Platelet Rich Plasma Injections.
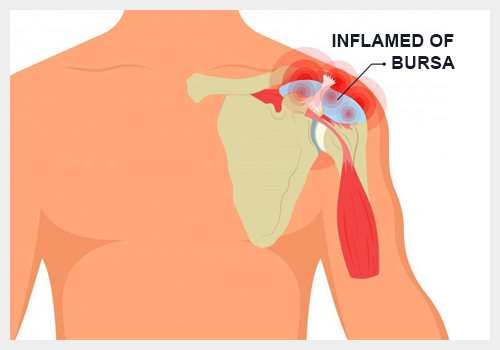
- The subacromial-subdeltoid bursa (SASD) is a potentially pain-sensitive structure of the glenohumeral joint. Located beneath acromion bone and deltoid muscle, inflammation in this empty space can be due to trauma, degeneration, systemic illness or overuse and can lead to impingement of supraspinatus muscle. When inflamed, a bursitis limits movements such as internal rotation, abduction and flexion. A dynamic ultrasound of shoulder can reveal bursitis and treatment is 100% non-surgical and holistic which includes medicines, electrotherapy, lifestyle modifications, exercises, diet and injections.