Neck Pain is a pain posteriorly anywhere between skull base and thoracic spine. It is often accompanied with shoulder and arm pain. Approximately 2/3 of the world population suffers from acute or chronic form of neck pain during their lifetime. It is common in all ages. Neck Pain is multifactorial in origin. Poor posture, bad ergonomics, lack of physical activity, neck sprains, anxiety, depression, stress, gadget use etc can all play a role. It can be a part of multisystem problems like Rheumatoid Arthritis, Ankylosing Spondylitis etc. At SAAOL Ortho Care, we take an integrative, multidisciplinary approach in curing your neck pain using an extensive armamentarium of treatment approaches. We encourage you to contact us today to get a quick and long lasting relief.
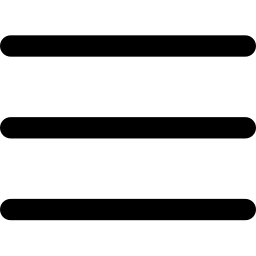
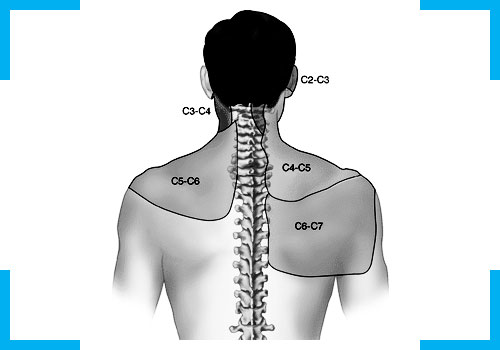
The neck (also known as cervical spine) is a part of a long flexible column, known as the spinal column or backbone, which extends through most of the body. The cervical spine (neck region) consists of seven bones (C1-C7 vertebrae), which are separated from one another by intervertebral discs. These discs allow the spine to move freely and act as shock absorbers during activity. Cervical Spine is a well-engineered structure that is remarkably strong and yet flexible, allowing neck to move in all directions. At each vertebral level (C1-C7), a pair of spinal nerves exit through small openings called foraminae (one to the left and one to the right) which serve the muscles, skin and tissues of the body and thus provide sensation and movement to all parts of the body. The delicate spinal cord and nerves are further supported by strong muscles and ligaments that are attached to the vertebrae.
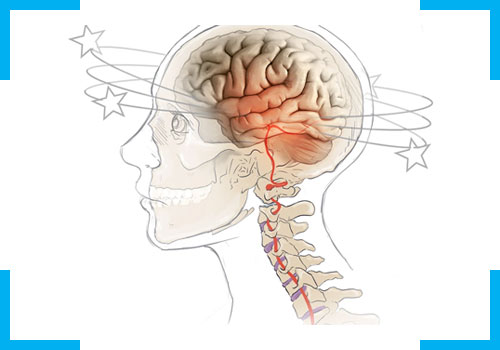
Cervicogenic vertigo is the false sense of motion that is due to cervical musculoskeletal dysfunction. It is believed that it occurs due to mismatch of signals to the brain which leads to dizziness and spinning of head. This can occue commonly post trauma, degeneration, inflammation, disk lesions or abnormally high muscle tone due to faulty posture. Cervicogenic dizziness is a clinical diagnosis. Testing may include cervical radiographs to rule out cervical osteoarthritis or instability. Treatment includes medications, rehabilitation, manual therapy, UST, PEMF, exercises and tender point injections using local anaesthetic, anti inflammatories or Botulinum toxin.
Cervical sprain or strain typically refers to acute pain arising from injured soft tissues of the neck, including muscles, tendons, and ligaments. It commonly happens after an injury or faulty posture during working or sleeping. Patient generally reports of neck pain which worsens with movement leading to extreme stiffness and tightness. Other associated symptoms can be dizziness, ringing in the ears, fatigue and patchy numbness in hands or arms. Diagnosis is mostly clinical but MRI can be done if an injury is suspected. Treatment involves medications (analgesics and muscle relaxants), early mobilization leads to favourable outcomes and thus electrotherapy, manual therapy and exercises are helpful, cupping, dry needling and interventional pain management.
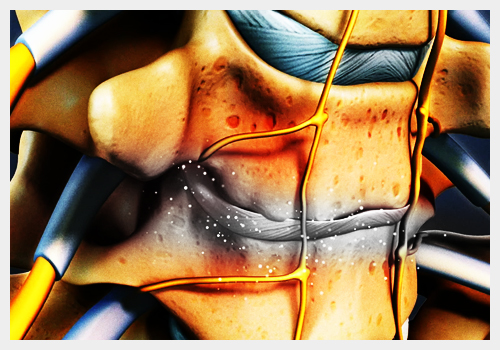
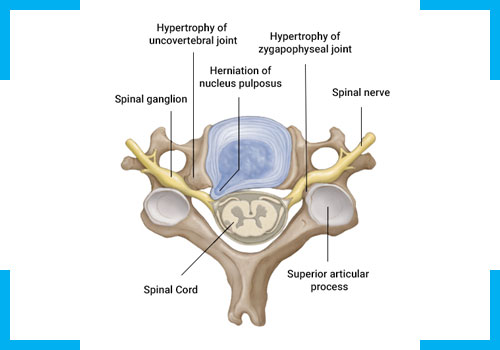
The term cervical degenerative disease encompasses a wide range of pathologic changes affecting all the components of the cervical spine that may lead to axial or radicular pain. The mechanisms underlying cervical degenerative disease are complex and multifactorial. Genetics, aging, and attrition to posture and metabolism may all play an important role. It is believed that disc degeneration results in altered, abnormal load distribution, which in turn leads to a cascade of structural changes that affect the various components of the spinal column. This leads to structural changes that may change spinal posture and stability and may compromise neural function. The pain is usually more severe in the upright position and relieved only with bed rest. Cervical motion, especially hyperextension and side bending, increases the pain. Treatment involves medications, manual therapy, electrotherapy, exercises, cupping, needling and interventions.
Cervical facet joints are paired diarthrodial structures located in the posterior portion of the spinal axis. These synovium-lined joints contain highly innervated joint capsules and allow mobility and stability to the head. Cervical facet arthropathy refers to any acquired, degenerative, or traumatic process that affects the normal function of the facet joints in the cervical region, often resulting in a source of neck pain and cervicogenic headaches and vertigo. Patients complain of pain in neck or back side of head which aggravates on extension and rotation. Treatment involves medications, manual therapy, electrotherapy, exercises, cupping, needling and interventions.
Cervical radiculopathy is characterized by signs and symptoms related to cervical nerve root dysfunction. The patient usually presents with neck pain that radiates into the arm. It can be associated with loss of motor function, sensory loss, or reflex changes in the affected nerve root distribution. The most common causes of cervical radiculopathy are cervical disc herniation (most commonly posterolateral) and cervical spondylosis (osteophytic spurs from the vertebral body, uncovertebral joint facet joint, or a combination) causing nerve root compression. Symptoms include Neck pain with radiation following dermatomal pattern which exacerbate on Cervical hyperextension and lateral bending or rotation ipsilateral to the pain, coughing and valsalva maneuver. Treatment includes medications, rehabilitation, UST, TENS, IFT, PEMF, Traction, lifestyle changes, exercises, cupping, needling, diet and cervical injections.
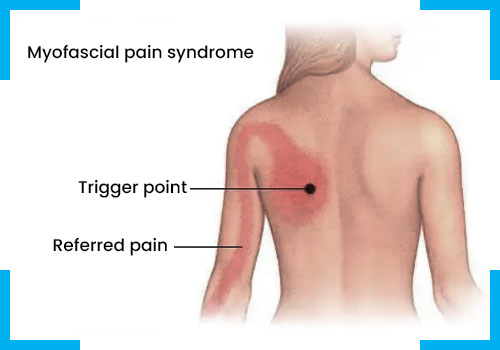
It is characterized by hyperirritable spot(s) in skeletal muscle that is associated with a hypersensitive palpable nodule in a taut band. The spot is painful on manual compression and can give rise to characteristic referred pain, referred tenderness, motor dysfunction, and autonomic phenomena. It can be multifactorial and have several causes like hypermobility or forward neck stooping, forward shoulder posture, repetitive stress injuries, excessive telephone and computer use, structural changes, hypothyroidism, calcium vitamin D deficiency etc. It is characterized by dull localized pain with worsens with activity and extreme tenderness. Treatment includes medications, rehabilitation, manual therapy, UST, PEMF, exercises and tender point injections using local anaesthetic, anti inflammatories or Botulinum toxin.